Sarah Knows Eyes
In case you’ve been living under a rock these past few months, you may have noticed a new trend in the world of Optics – everything’s gone round!
During my 14 years in practice, every now and then you would encounter somebody looking for a “John Lennon” – the round frame is synonymous with the icon, who was rarely seen without them.
.jpeg)
However, I wouldn’t exactly have said they were an en vogue choice? Until now. Sunglasses, Ophthalmic frames, you name it, round is in and here is the proof…
Back in December, Tatler published this article, confirming my suspicions that a new trend was about to hit:

Cue, the ‘big brands’ jumping aboard the round frame train in their glossy advertisements:

And follow suit a plethora of celebrities rockin’ the round frame:

One of the biggest drivers of this new trend has been Dior’s “So Real”, the “new Wayfarer” according to March’s Glamour magazine (they’re featured twice in the edition!):


And since Rihanna featured in their ad campaign...
.jpg)
…the A-listers have certainly been clamouring to be seen in its multitude of colour combinations:

You know a trend is firmly cemented when they are used in non-Optical related ad campaigns:
.jpg)
My favourite wearer of the round spectacle frame has to be McFly’s Tom Fletcher, who has the style in several colours and isn’t afraid to bear them all over his Instagram. ❤️ you Tom!

If you read my blog post “The Significance of Face Shape when Choosing Glasses”, you’ll know that this trend is perfect, as round spectacles tend to suit most face shapes (oval/long/square/heart), possibly with the exception of those who have a more rounded face shape, which can serve to emphasise ithe fact. However, as I always say never be afraid to try them on, because you never know, you might just look awesome in them!?
If you have succumbed to the round trend please send me a picture (preferably of you wearing them!) as I’d love to see them! Share them on my Facebook or Twitter page using the hashtag #roundframes – thank you!
Write comment (1 Comment)
.jpg)
Believe it or not, this post is actually one of the reasons I first started SarahKnowsEyes, so I’ve had it in mind for quite some time! In fact, it was whilst watching Edgar “Pitbull” Davids, playing for the RoW team during SoccerAid 2014 (I was only watching because Danny from McFly was playing for England!), that it occurred to me that many people might be wondering why he wears goggles when he’s playing football. It’s because he suffers from glaucoma, and whilst a person newly diagnosed with this condition may feel like it’s the end of the world, Davids is proof that it's absolutely not – he is after all an international footballing legend! And so SarahKnowsEyes was born, created as a platform for me to impart just this sort of knowledge, and because I’m fortunate enough to be in a position to do so. (I just had to wait until now for this particular post, as SoccerAid is a biennial event! And fortunately Edgar Davids is playing again!)

So what exactly is glaucoma? The eyeball contains a fluid called aqueous humor which is constantly produced by the eye, with any excess drained though tiny little tubes. If for some reason, this fluid cannot drain properly, pressure builds up within the eye, this is known as the 'intraocular pressure'. Glaucoma is actually a group of eye diseases in which the optic nerve (which connects your eye to your brain) and the nerve fibres from the retina (the light-sensitive nerve tissue that lines the back of the eye) are damaged by this intraocular pressure. This may be because the pressure is higher than normal, or because the nerve is more susceptible to damage from pressure. Glaucoma often affects both eyes, usually to varying degrees and one eye may develop glaucoma quicker than the other.
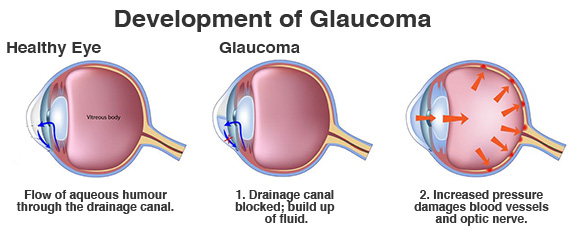
/via www.londoneyespecialists.co.uk
There are four main types of glaucoma: -
- Chronic open-angle glaucoma – this is the most common type and develops very slowly.
- Primary angle-closure glaucoma – this is rare and can occur slowly (chronic) or may develop rapidly (acute) with a sudden, painful build-up of pressure in the eye.
- Secondary glaucoma – this mainly occurs as a result of an eye injury or another eye condition, such as uveitis (inflammation of the middle layer of the eye).
- Developmental glaucoma (congenital glaucoma) – a rare but sometimes serious type of glaucoma which occurs in very young children, caused by an abnormality of the eye.
Anyone can develop glaucoma, however, there are people at a greater risk, such as if you are: -
- Aged over 40.
- Very short-sighted.
- Of African or Caribbean origin (or with very dark coloured eyes).
- Closely related to someone with glaucoma, as it can be hereditary. (In fact, if one of your parents or children, or a brother or sister, has glaucoma, and you are over 40, the NHS will pay for your eye examination.)
Some people naturally have pressure that is above normal range, but this pressure does not cause any damage to their eyes. Although they do not have glaucoma, they may still be more likely to develop it.
Because you often cannot feel the pressure in your eyes, and damage occurs slowly, you may not even know you have glaucoma until a great deal of damage has already been done. If you have glaucoma but do not treat it, your eyesight will gradually get worse….

This damage is irreparable, and you could eventually go blind! Remembering however that this is supposed to be an "upbeat" blog post – the good news, is that treatment as simple as eye drops, may stop it getting worse! This is why early detection is absolutely vital. Optometrists recommend that most people should get their eyes tested every two years, however if you are at risk of developing glaucoma, they may recommend more frequent NHS eye examinations.
For more information about how glaucoma is detected, click here.
What will happen if you do get diagnosed with glaucoma? Unfortunately, there is currently no cure for glaucoma, and although any existing damage will most likely be permanent, its progression can effectively be halted. If your Optometrist suspects that you may have glaucoma, he or she will refer you to an Ophthalmologist. If you do have glaucoma, you will be given eye drops to use every day, these will reduce the pressure within the eye(s) and help control the build-up of fluid. Don’t worry, they won’t hurt!

(Love this picture so much, I just had to use it again!)
Because you won’t feel different in any way, you won’t know if the treatment is working, but your sight could get much worse if you stop the treatment, therefore it is very important that you, a) attend your follow-up appointments, and b) keep using the drops, even if you can’t tell if they’re helping. If you find it hard to use eye drops, there are special bottles available or holders to make it easier. In a small number of cases, an Ophthalmologist may recommend that you have an operation, called a trabectome, to help drain the fluid.
So why does Edgar Davids wear goggles when he’s playing football? To prevent his eyes from a traumatic injury that could further raise his intraocular pressure. The point being that it doesn’t stop him doing what he loves and making a very successful and lucrative career from it! Ever wondered why U2 frontman Bono always wears sunglasses?

..because he too has glaucoma! Now, I have to admit that I had to research this one – apparently, loss of contrast sensitivity, problems with glare, and light sensitivity are some of the possible effects of glaucoma that may interfere with your day-to-day activities, with some glaucoma medications exacerbating the problem even further. Sunglasses are an easy solution that can make life more comfortable, while also providing critical protection from the sun’s damaging ultraviolet (UV) rays when outdoors. See? Glaucoma hasn’t prevented Bono from being a world famous rockstar either?!
In fact, Bono is so rarely seen without his trademark sunglasses, that he was the perfect “celebrity ambassador” to front Revo’s brand campaign: “Buy Vision, Give Sight”. The legendary rockstar has created his own line of luxury sunglasses for the brand – for which he also features in their advertising campaign – $10 from the sale of every pair will go towards helping those fighting for their sight around the world. The creative collaboration hopes to raise $10million to improve access to eye screening, prescription glasses and eye health care in under-resourced communities, in a bid to combat vision impairment and unnecessary blindness.
In a statement on Revo’s official website, Bono said:
“The ‘Buy Vision, Give Sight’ campaign is a very personal one for me. Thanks to good medical care my eyes are okay, but tens of millions of people around the world with sight problems don’t have access to glasses, or even a basic eye test. Poor eyesight may not be life-threatening, but it dramatically affects your life and your livelihood if you aren’t able to fix it.
Sight is a human right and the ‘Buy Vision, Give Sight’ initiative will help ensure millions of people have access to the eye exams and glasses they need to see.”
What a great guy huh?
Actress Whoopi Goldberg also suffers from the condition….

Well, hopefully this has proved that being diagnosed with glaucoma really isn’t the end of the world and if it’s diagnosed early and treated effectively, you should be able to lead a perfectly “normal” life, and do whatever you want to do (within reason – bungee jumping is probably ill advised?!). However, as demonstrated in this and countless blog posts before it – early detection is the key and subsequently regular eye examinations are a must! So, if you haven’t had your eyes tested for two years or more, do so, pronto, especially if you have a parent, child, brother or sister with glaucoma! You’re not doing yourself any favours by procrastinating! Here endeth the lecture.
Write comment (5 Comments)
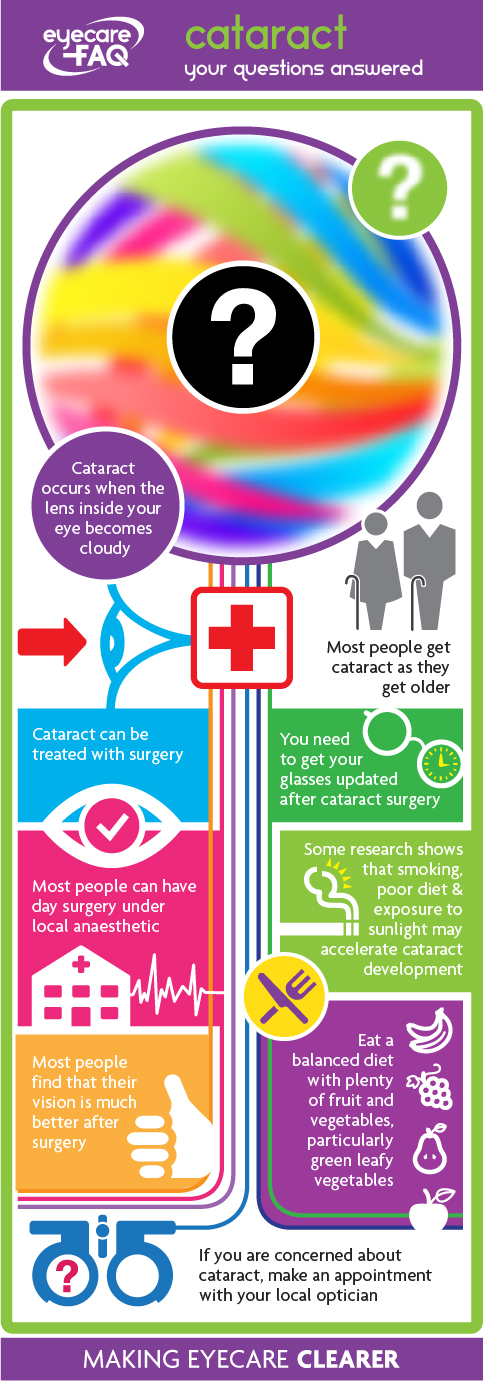
Last month, having possibly scared the living daylights out of anyone facing the prospect of cataract surgery, I thought I’d better try to redeem myself, by pointing out that it’s really not THAT bad! Medicine has indeed moved on significantly since the 18th century and, certainly in the Western world, the brutal “couching” is by far a thing of the past. Today, surgeries in which cataracts are removed and the lens replaced are among ophthalmology's (and medicine's!) most successful procedures.
Firstly, let’s start by explaining what exactly a cataract is. As briefly touched upon in my blog “The Truth About UV Protection”, a cataract is the opacification (clouding) of the lens in the eye.
.jpg)
I’m a little ashamed to admit, but it wasn’t until researching this blog that I realised just how many different types of cataract there are! The most common is ‘age-related’, caused by prolonged exposure to ‘incident’ (present in the environment) ultraviolet radiation. Most people will develop cataracts as they get older – more than one in two people aged 65 and older have some signs of cataract, and they are present in almost everyone over 75.
Some people are born with them – these are known as ‘congenital’ cataracts. A trauma to the eye can cause a cataract, as can certain metabolic disorders, such as uncontrolled diabetics, galactosemia, Wilson disease, and Myotonic dystrophy.
NHS guidelines concerning referral for cataract surgery are very prudent and basically tie-in with the DVLA’s driving standards: -
“You must be able to read (with glasses or contact lenses, if necessary) a car number plate made after 1 September 2001 from 20 metres.
You must also meet the minimum eyesight standard for driving by having a visual acuity of at least decimal 0.5 (6/12) measure on the Snellen Scale (with glasses or contact lenses, if necessary) using both eyes together or, if you have sight in one eye only, in that eye.”
/via https://www.gov.uk/driving-eyesight-rules
As result, we wait until the cataracts are “ripe”, i.e. the Optometrist can no longer correct your vision to comply with these driving standards. There are exceptions to this rule, for instance, a patient who experiences disabling glare due to cataract when driving may still achieve a visual acuity of better than 6/9 under ideal conditions of illumination, or where anisometropia is causing symptoms. On occasions, cataract surgery may be performed primarily to aid the management of other eye conditions, for instance to facilitate surveillance or treatment of diabetic retinopathy or to improve intraocular pressure control in primary angle closure glaucoma.

Just kidding!!!
The procedure itself is usually done under local anaesthetic. You will be awake, but the ophthalmologist will make sure you do not feel the area around your eye. You should (hopefully!) hear the ophthalmologist explaining what he/she is doing, and you may see some vague movements around your eye. The ophthalmologist will make a tiny cut in your eye to remove the cataract - they basically blast the clouded lens with ultrasound and then suck out the remnants. They will normally then insert a plastic replacement lens so that you can see clearly again. This will usually take between 15-45 minutes. The procedure generally does not require stiches, but your eye will be covered to protect it from knocks after the operation. You will be allowed to go home the same day, but you should have someone go with you to the appointment, and to look after you for the following 24 hours. You must not drive.
Now, I absolutely hate the thought of somebody poking about in my eyes, I’d rather have a Ceti eel crawl in my ear, but having been working in Optics for 14 years now (yes, I’m THAT old!) I have seen many a patient before and after having their cataracts done, and they all assure me that there is absolutely nothing to be nervous about. And that the results are amazing!
If any of you are waiting to have your cataracts done, I hope this blog post has gone, even just a little way, to putting your mind at rest, but as always, if you have any questions, or would like any further information about this topic, then please do not hesitate to contact me using the “Ask Away” link above.
Write comment (0 Comments)Page 4 of 16